By Paul Derienzo
Top-level federal researchers and bureaucrats, as well as grass-roots activists in drug-ravaged urban communities, have discovered ibogaine, the controversial drug that advocates tout as an “addiction interrupter” and one scientist calls a “probe into the inner workings of the human brain.”
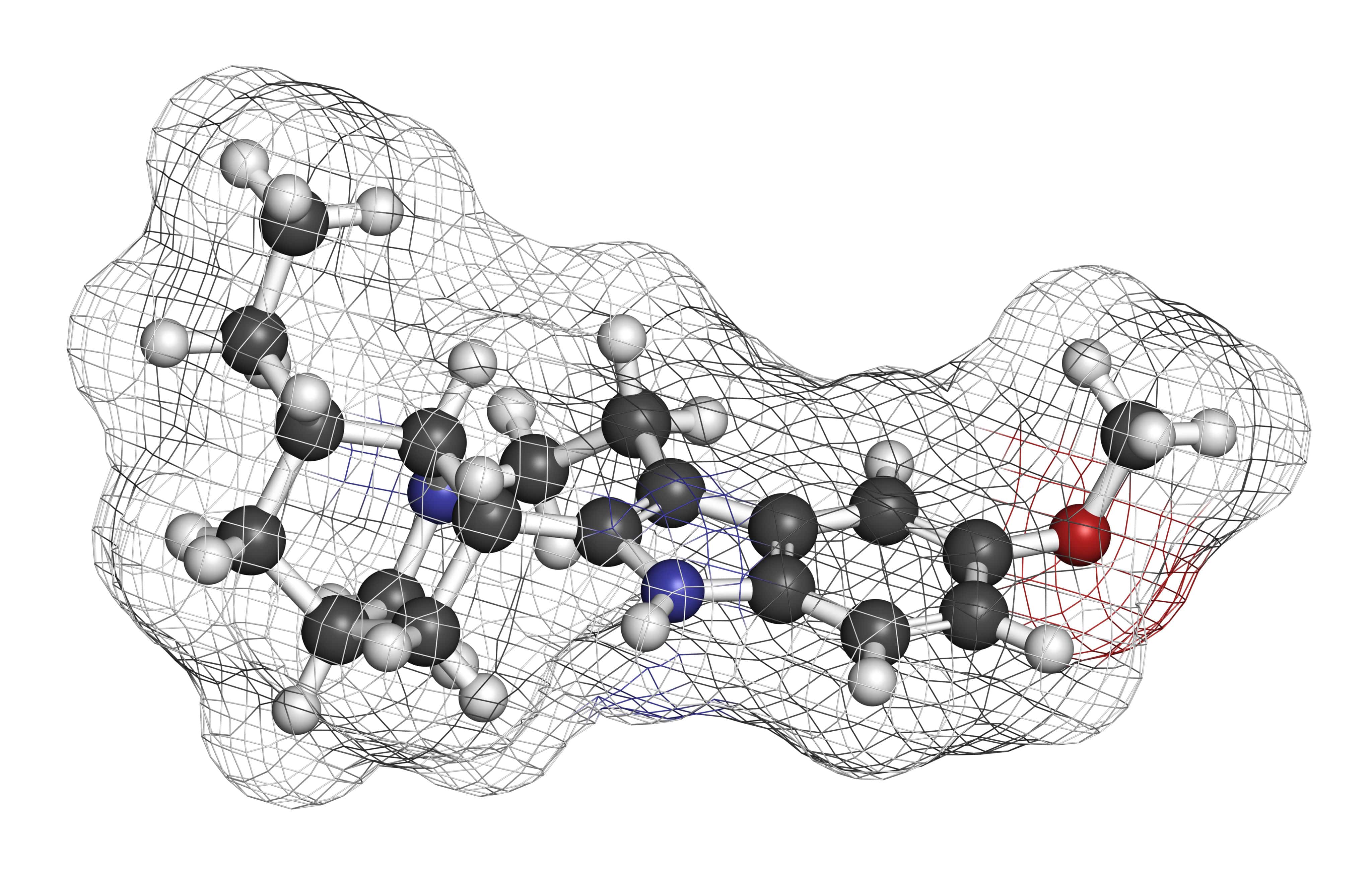
Derived from iboga, an hallucinogenic plant of the West African rainforests, ibogaine is illegal in the USA. But addicts have been successfully treated with the drug in programs run overseas by private outfits, which are now pressuring the federal government to legalize the treatment.
The ibogaine controversy was aired at a March 8 conference in the Washington suburbs called by the National Institute on Drug Abuse. Amidst heated debate between pro and anti-ibogaine factions, Frank Vocci, deputy director of NIDA’s Medications Development Division, expressed misgivings over human ibogaine testing conducted in Europe, Israel and Panama, and the reliance on “anecdotal evidence” of its efficacy in interrupting heroin and cocaine withdrawal symptoms. He concluded, however, that ibogaine research is “here to stay.”
Dr. Carlo Contoreggi of NIDA’s Division of Intramural Research said “even if ibogaine is slowed down, it’s too late to stop it. They know it works. NIDA views it as a fascinating window into the human brain, a probe to the farthest reaches of addictive behavior.”
Howard Lotsof, who heads NDA International, the company that holds the ibogaine-therapy patents, summarized the 60 treatments his group has performed, mostly in Holland. Lotsof characterized the drug’s effectiveness as “15 percent success, 15 percent failure, with the length of interruption in everyone else falling somewhere in between on a bell curve.”
Among the strongest ibogaine advocates at the conference was Dr. Deborah Mash of the University of Miami Medicine School’s Neurology Department, who is conducting the first FDA-sanctioned human testing (“FDA Approves Ibogaine Research on Humans,” Jan. ’94 HT). Mash has identified an ibogaine metabolite, 12-hydroxy-ibogamine, which is active at opiate receptor sites in the cerebellum.
According to one highlevel NIDA official, her discovery is among the most significant in the study of addiction.
But drug-research consultant Dr. Peter Hoyle, who was involved in the controversial approval of the AIDS drug AZT, is an adamant ibogaine critic. He said he doesn’t think enough preclinical work has been done to support human trials. He said the mechanism of ibogaine’s action is still unclear, and raised the specter of ibogaine toxicity, based on massive overdosing of laboratory dogs and rats.
Others countered that despite the high doses—far greater than the doses used on humans—only one of the laboratory animals died. Dr. Mark Molliver of Johns Hopkins University, who first published results showing brain damage in rats given massive doses of ibogaine, said studies in monkeys showed only minor evidence of cell damage.
Mash dismissed reports of cell damage. Her own primate studies show absolutely no cell damage. In the conference’s most dramatic moment, she presented an actual human brain, of a heroin addict who died a month after she had received an ibogaine treatment in Panama. The patient died in Miami, where she had gone for a medical exam after experiencing vomiting and diarrhea. The local medical examiner who did the autopsy was an associate of Mash. According to the autopsy report, the brain showed no damage to the cerebellum area where ibogaine is active.
One source close to federal researchers says there are powerful forces arrayed against ibogaine inside the drug-policy bureaucracy. These forces are said to be centered around the methadone establishment.
Methadone is a heroin substitute invented in 1930s Germany and initially called Dolophine after Nazi leader Adolf Hitler. Government-funded clinics coast-tocoast dispense it to addicts in “maintenance” programs aimed at controlling addiction. According to the source, there are some scientists who have built their careers on methadone research and are fighting toothand-nail against ibogaine. A “methadone mafia” is said to be entrenched in the drugpolicy bureaucracy.
On March 4, mere days before the Washington conference, 400 people jammed a forum on ibogaine in New York City’s African American community of Harlem. The forum, jointly organized by the Black Coalition on Drugs and the African Descendants Awareness Movement, was held at a community center near the mosque where Malcolm X was once minister. Among the scheduled speakers were two former Black Panther political prisoners.
After 19 years in prison, Dhoruba binWahad was recently cleared of charges linking him to the shooting of two police officers in 1971. Dhoruba had been raiding South Bronx drug locations that operated with the connivance of corrupt officers and then publicly dumping the drugs into sewers.
Dhoruba couldn’t make the forum because of a delay in his flight from Ghana, but speaking in his place was Eddie Ellis, also a former Panther and a veteran of 25 years incarceration.
Through a letter from Dhoruba, the Black Coalition on Drugs voiced full support of ibogaine, stating that the drug should be made available to the estimated 800,000 heroin and cocaine addicts in the USA. Rommel Washington, a Harlem Hospital social worker who has observed several ibogaine treatments, led the audience in chanting “Ibogaine is life!”
Questions about ibogaine’s pharmacological properties were fielded by Dr. John Morgan of City College of New York, who recounted reports from nearly 80 addicts who have received ibogaine _ treatments in Holland, Panama and other countries. He says it has been shown to alleviate morphine withdrawal in preclinical tests and anecdotal evidence. But the doctor also cautioned the gathering that some scientists were actively trying to halt human ibogaine testing.
Howard Lotsof called on the forum participants to increase the pressure on NIDA and local elected officials such as Rep. Charles Rangel, a hard-line Drug Warrior who once chaired a congressional subcommittee on narcotics.
Natural-healing advocate John Harris, who appears regularly on local radio, spoke on iboga’s historic use in African rite-ofpassage ceremonies. Drawing a parallel, he advocated involvement of the addict’s family and friends in ibogaine treatment.
Longtime organizer Dana Beal, veteran Yippie and fixture on the marijuana-activist scene, spoke in support of a “harm reduction” approach combining ibogaine with medical marijuana and long-term counseling as a holistic anti-addiction strategy. Beal says ibogaine is best understood through study of West Africa’s Bwiti spiritual tradition, in which practitioners under the influence of iboga are said to meet with their ancestors in a lifetransforming experience.
Despite the hope many participants held for ibogaine, the impassioned question-andanswer session indicated that many saw a contradiction between the white medical establishment’s control of drug policy and an African-American community determined to explore an addiction treatment derived from an African rainforest plant.
Organizer Brother Shine asked rhetorically if black Americans can depend on the medical establishment to treat ibogaine research fairly—and answered his own question by urging grass-roots involvement to ensure that the drug ultimately comes under the control of the local communities hardest hit by addiction.
Read the full issue here.
Read the full article here